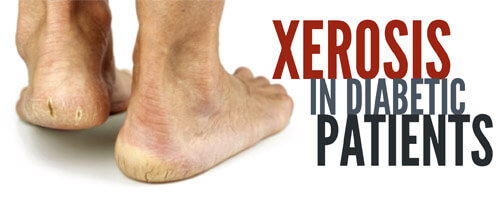
Diabetic wound management requires awareness, including knowing the signs and progression of xerosis – an abnormal dryness of skin.
Patients with diabetes are prone to dry skin, particularly when blood glucose levels are running high. And as a clinician, one of the most common types of skin conditions you will see in your diabetic patients is xerosis, which is an abnormal dryness of the skin. This is just one reason why clinicians should routinely inspect the feet of diabetic patients.
According to research, 82.1% of patients with diabetes had skin with dryness, cracks or fissures, which serves as a predictor of foot lesions. In addition, an unpublished survey of 105 consecutive patients with diabetes revealed that 75% had clinical manifestations of dry skin. This serves as further evidence that xerosis in diabetic patients is a threat to foot ulcers, and the more we know about the condition, the better we can treat and heal our patients.
The Signs
The most common characteristics of xerosis include excessively dry, rough, uneven and cracked skin. Other signs include:
- Possible raised or uplifted skin edges (scaling), desquamation (flaking), chapping, and pruritus.
- Excessive dryness and scaling on the heels and feet.
- Possible fissures (linear cracks in the skin) with hyperkeratotic tissue.
Progression and Patterns
The progression of xerosis follows a defined pattern that begins when the skin becomes dry and rough, with pronounced skin lines. As the condition progresses, you’ll see the development of superficial scaling, with fissuring and erythema. In severe cases, a crisscrossing pattern with superficial scaling is present. The skin becomes less elastic and loses both its flexibility and its ability to withstand trauma, which may result in skin breakdown and subsequent infection.
Causes
A number of conditions contribute to the onset of xerosis in diabetic patients, including the loss of natural moisturizing factors and moisture from the stratum corneum and intercellular matrix of the skin. Additionally:
- Sebaceous and sweat glands normally maintain skin lubrication and control the oil and moisture in the foot, but they become atrophied when autonomic neuropathy occurs.
- Corneocytes (cells that make up the top layer of epidermis) are aligned parallel to each other in normal skin; xerosis causes structural changes to these cells and disrupts the surface, resulting in a rough epidermal surface.
- The dryness is due to the redistribution of blood flow in the soles of the feet by persistent and inappropriate dilatation of arteriovenous shunts. This activity diverts blood away from the skin surface. When this occurs in combination with alterations in the elasticity of the skin (due to nonenzymatic glycosylation of structural proteins and glycoproteins), the skin splits, creating portals for bacteria to enter.
Treatment
Once you see initial signs of xerosis in your patients, what should you do? Start by applying an agent to the feet every day in order to maintain skin moisture, such as an emollient lotion or cream. Use moisturizers that contain urea or lactic acid.
- Urea works by enhancing the water-binding capacity of the stratum corneum. Long-term treatment with urea has been demonstrated to decrease transepidermal water loss. Urea also is a potent skin humidifier and descaling agent, particularly in 10% concentration.
- Lactic acid (in the form of an alpha hydroxy acid) can accelerate softening of the skin, dissolving or peeling the outer layer of the skin to help maintain its capability to hold moisture. Lactic acid in concentrations of 2.5% to 12% is the most common alpha hydroxy acid used for moderate to severe xerosis.
- Examples of products with urea or lactic acid include Atrac-Tain Cream, Eucerin 10% Urea Lotion, Lac-Hydrin 12%, and AmLactin Foot Cream Therapy.
Additionally, it’s important to avoid:
- Products that contain alcohol – because they evaporate, and their drying action compounds the original problem.
- Petroleum-based products, because they seal the skin surface and prevent what little lubrication is made from evaporating. These products don’t penetrate the surface of the skin and don’t replace skin moisture.
Patient education
As always, part of our job is to continuously educate patients and their family members or caretakers. When it comes to your patients suffering from xerosis, make sure they know to:
- minimize bathing to no more than once a day (or even every other day)
- use cool or lukewarm water
- pat – don’t rub – to dry the skin
- avoid harsh soaps
- avoid lotions with dyes or perfumes
- ensure skin moisturizers are applied appropriately and at the right frequency
What do you think?
Knowing the signs of xerosis and how to treat it is crucial for diabetic patients. Have you had experience with this condition, and are there any specific techniques, treatments or products you find most effective? And what are the biggest challenges you face when it comes to this particular type of wound management? We would love to hear about and learn from your experiences! Please share your stories below.
Wound Care Education Institute® provides online and onsite courses in the fields of Skin, Wound, Diabetic and Ostomy Management. Health care professionals who meet the eligibility requirements may sit for the prestigious WCC®, DWC® and OMS national board certification examinations through the National Alliance of Wound Care and Ostomy® (NAWCO®). For more information see wcei.net.
What do you think?