As a wound care nurse, you teach your patients how to care for their wounds, including a colostomy.
You teach them as they observe treatments you provide, such as ostomy care, while they are at a clinic.
It also includes orally reciting your care as you carry out treatment and direct the patient. This empowers them to understand what is required for appropriate personal care.
You also might write down instructions and diagrams about required treatment that patients can take home and reference.
The teach-back method of patient instruction incorporates both of these approaches. This is when you have the patient repeat back what you instruct and demonstrate the care you described.
Any patient teaching also requires that the patient comprehend your:
- Demonstration of care
- Verbal instructions
- Ability to carry out the treatment
Patient’s ability to perform ostomy care
In the following case, the key issue was the patient’s ability to carry out her own ostomy care.
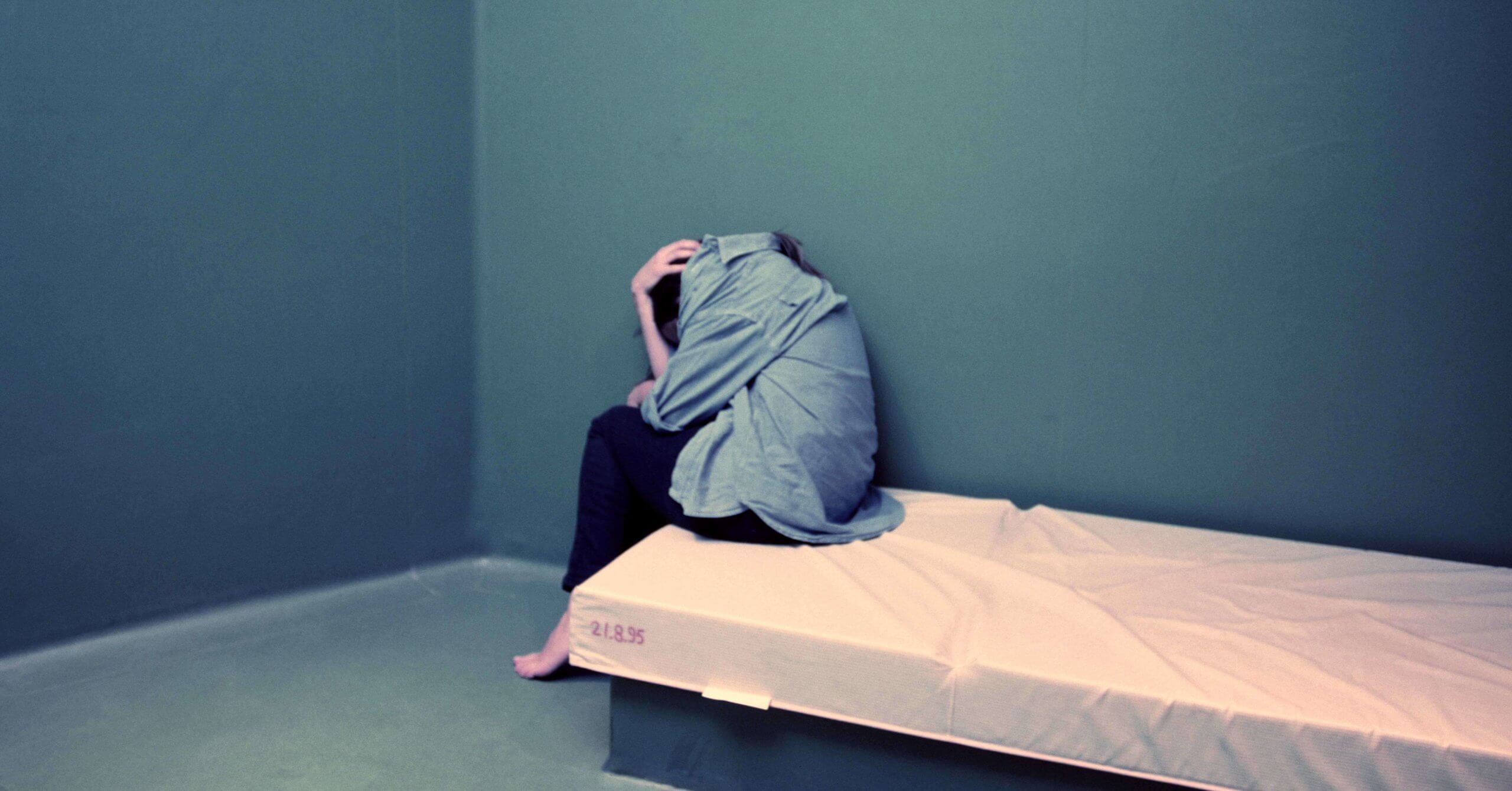
A medical team was caring for a female patient, age 61, at a behavioral health center. Before she was at the center, the patient had been in jail and lived in a nursing facility.
She was diagnosed with a “depressive disorder, memory issues and declining executive functioning,” indicating a “major neurocognitive disorder.”
In addition, the patient had a number of serious physical conditions, including untreated Hepatitis C, chronic kidney disease and cancer.
Eight years ago, her cancer resulted in the surgical removal of part of her bowel and an ostomy.
A hearing to commit her to the state health authority for up to 180 days was granted because of her mental illness. She was not able to complete her basic care alone.
The patient appealed that decision.
Patient’s condition prior to appeal
She was admitted to a hospital for care because of her condition. Then, a CT scan revealed the ostomy site had an infection or inflamation.
Despite some improvement while in the hospital, one of her physicians believed her ostomy care needed improvement.
Notes by the nurses who cared for the patient detailed her attempt to place foreign objects into her stoma.
In addition, administering medications to the patient was difficult. A nurse would give her medications, but the patient did not recall taking them. This would result in patient agitation.
Also problematic was the patient’s inability to keep the ostomy site sanitary by using gloves. She also would often poke and use abrasive things on it.
Appellate court ruling
The appellate court carefully reviewed the evidence and testimony during the commitment hearing. The testimony of a physician who cared for her in the hospital was particularly important.
In addition to testifying to the above behavior of the patient, he said if the ostomy site was not properly cared for she was at risk of infection and obstruction.
Plus, he emphasized the need for follow up with a consistent medical provider.
He believed the patient’s ability to care for herself was “lesser than the degree of care which her medical issues require.”
The physician also said that if the patient was released, she would likely drink alcohol. As a result, drinking would make her more depressed and less able to care for herself.
The doctor also said if she did not eat properly, she might become obstructed, with no output from the ostomy bag. A fever would follow and bacteria would enter her bloodstream causing her to become septic and go into organ failure.
The appeals court opined that this case was a “close case.” They discussed whether commitment was appropriate, based on the patient’s inability to care for her ostomy site because of her mental disorder and memory lapses.
The commitment ruling of the trial court was affirmed because the patient was unable to provide her basic personal needs. This ruling protects her from serious physical harm because of lack of proper care in the future.
Involuntary commitment
This case illustrates an involuntarily commitment of a mentally ill individual to a mental health facility. This is because the patient was unable to provide for her basic needs.
Under state laws, the patient’s inability to provide proper ostomy care compromises her “safe survival” in the near future.
The power of a state is based on its parens patriate (parent of the country) authority to intervene on behalf of a person who cannot act in his or her own best interests.
Involuntary commitment is not something that is easily undertaken by any court. Nor should it be something easily undertaken because of a person’s inability to provide self-care.
Ramifications include:
- Stigma of being involuntarily committed
- Loss of liberty/freedom
- Questions about whether forced treatment helps someone with self-care
Takeaways for your wound care practice
However, when you observe a patient is unable to care for his or her ostomy — or any other wound — you need to raise this concern with the wound care team.
In doing so, you advocate to start the process to obtain the wound care required for your patient.
Factual, accurate and complete documentation in the patient’s medical record is important. Your notes should include:
- Patient teaching interactions
- Condition of the ostomy site
- Patient’s follow-through on subsequent visits
Sharing your concerns with the wound care team does not always result in involuntary commitment. Other options include seeking care help from:
- Family members (if present)
- Home health care (if the patient is living on his or her own)
- Required care provided and monitored by a staff member versed in wound care at a group living facility
If commitment is the only option, you may need to testify at the hearing about your experiences with the patient. The court will ask about details regarding the patient’s ability to provide personal ostomy care.
You can learn more about your state’s requirements for an involuntary commitment here. This will help you understand what is required if a patient cannot provide personal wound care.
Take our course on Ostomy Management.
What do you think?