Retained surgical bodies in a patient postop is not an unfamiliar occurrence.
One literature review indicated that with more than 28 million operations in the U.S. nationwide, 1,500 estimated cases per year of retained surgical bodies left in patients take place.
In the 2016 case of Thompson v. Mangham Home Care, Inc., who left gauze in a patient’s surgical wound was at issue.
The patient saw her primary care physician for boils/sores on both of her buttocks in 2008.
The primary doctor prescribed antibiotics without success, and the patient was referred to a general surgeon who treated the condition with antibiotics and warm soaks.
The condition continued and the general surgeon recommended surgery and referred her to a surgeon in a “surgeon’s group” (practice).
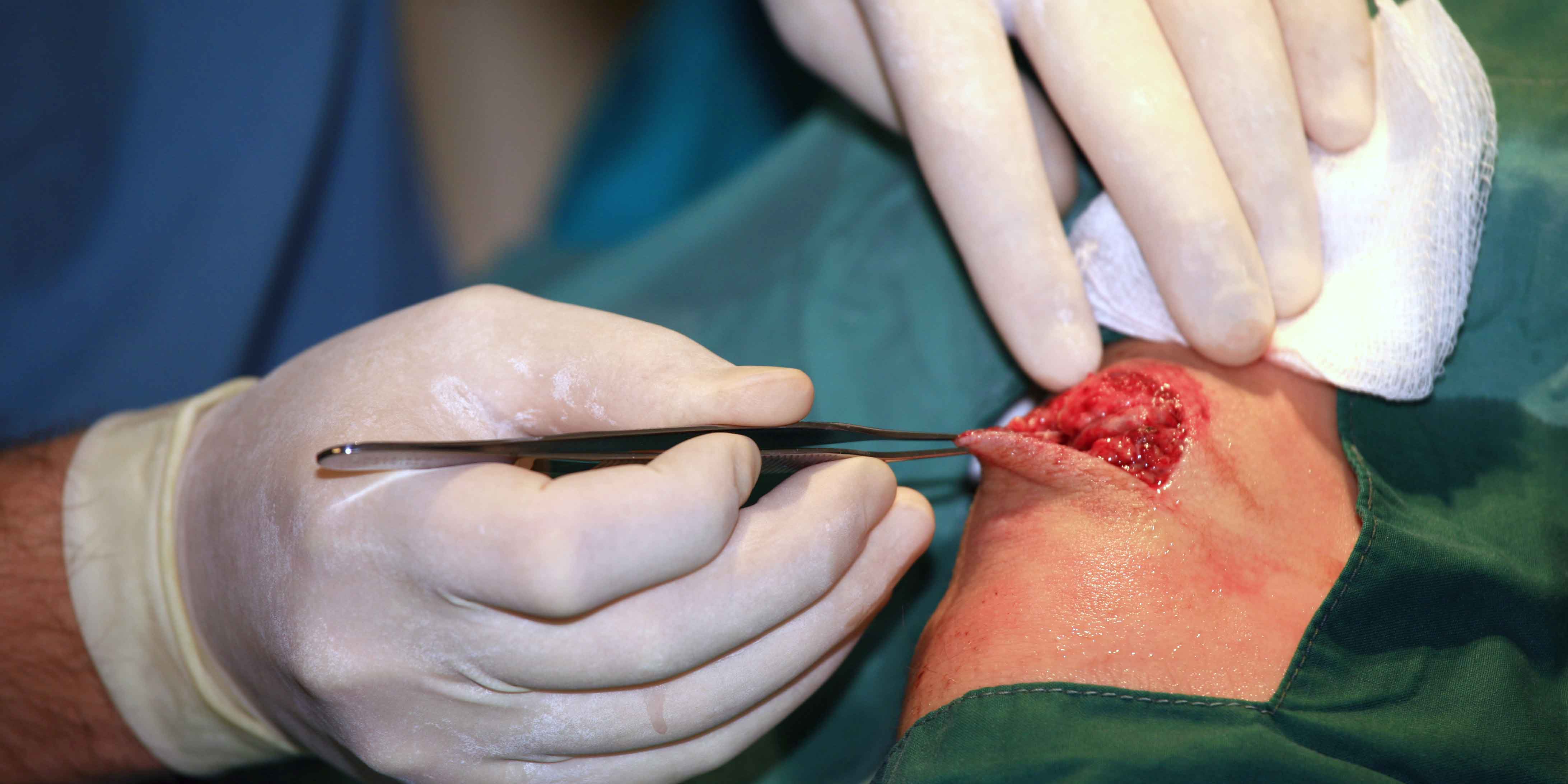
In 2009, the surgeon “surgically excised” the boils on both buttocks. His operative note stated he found a “sinus tract” in the left buttocks, made an incision, and debrided the scar tissue from the tract. He also debrided the right buttocks.
His operative notes and that of the circulating nurse stated the wounds were packed with ½-inch-wide gauze. The patient was discharged that day to her home.
The surgeon ordered daily wound care that required a home health nurse to:
- Remove the old gauze from each surgery site
- Clean each site
- Replace the gauze
- Bandage the wounds
A nurse did so the day after surgery. For almost a month, different nurses provided the same treatment except for two times when the patient saw the surgeon in his office, and he performed the treatment there.
The last time the patient saw the surgeon in his office, she was told both the wounds were closed and healed.
Wound complications arise
The left wound re-opened, and the patient returned to the surgeon’s office. He placed some gauze in the wound.
The patient removed this gauze several days later. No one else treated the wound, which periodically opened and closed for about seven months when the surgeon did a second surgery on the left wound.
No gauze was inserted. Rather, the surgeon stitched the wound closed. The stitches were removed by the surgeon 17 days later, and the surgeon told the patient the wound was healed.
The patient was involved in a car accident after her last visit to the surgeon.
When a CT scan was ordered, the radiologist noted a “sinus tract.” The wound re-opened and she was told to return to the surgeon, who did the surgery.
The surgeon, concerned about a possible diagnosis of cancer because of recent tests, referred the patient to a colorectal surgeon.
Surgery was scheduled, and during the procedure, the colorectal surgeon “found and removed from the wound a strip of 1/4-inch gauze” that was 11 inches in length.
After this surgery, the patient had no further problems with the wound.
Patient files lawsuit
After following required procedures for filing a medical malpractice suit, the home health care agency and hospital where the first surgery took place settled with the patient. Her claim against the surgeon and his insurer for damages survived.
A bench trial was held, and the judge issued a written opinion that the plaintiff (patient) proved by a preponderance of the evidence that the surgeon had negligently left gauze — retained surgical bodies — in the wound during surgery in 2009.
The patient was awarded $14,276.51 in medical expenses and $125,000 in general damages.
Additional damages in excess of $100,000 were assessed to the Patient’s Compensation Fund (a state statute). The fund filed a motion to intervene, and the motion was granted.
The surgeon, his insurer and the fund appealed the bench trial judgement.
Appellate court decision
After a careful review of the bench trial evidence, including the patient’s expert witness testimony, the appellate court held that because of the depth at which the gauze was found by the colorectal surgeon, it would be unlikely that a home health nurse or other person could have placed it at that location.
The surgeon who operated on the patient in 2009, therefore, breached the standard of care by leaving gauze in the patient’s wound and not removing the retained surgical body when he saw her in 2010.
Moreover, the testimony of the medical witnesses — except for the surgeon and his expert witness — was that the patient would have needed to be under anesthesia for the gauze to be placed at that depth.
A radiologist expert opined that a CT scan taken in August 2010 showed a mass in the exact location where the colorectal surgeon found the gauze and further testified that he “was confident” the gauze was present in the patient’s body in August 2010.
The defendants also argued that res ipsa loquitor (“the thing speaks for itself”) was improperly applied to the case. In this instance, the surgeon was the only one who had control over the surgery and gauze placement, and the patient could not have contributed to the injury.
The appellate court held that the surgeon and other defendants did not meet their burden of proof that this doctrine did not apply.
The judgment of the trial court was affirmed, and costs of the appeal were assessed against the physician, his insurer and the intervener, the fund.
Key takeaways on retained surgical bodies
Many healthcare providers were involved in the care of this patient. A careful analysis of each one’s conduct was needed to determine who left the gauze in the patient and who was legally liable for the retained surgical bodies.
If you are involved in packing a patient’s wound, either as a nurse or as a surgeon doing so after surgery, certain guidelines should be kept in mind.
They include:
- The use of packing materials requires accurate documentation as to where located, the size or number of material used, depth of the material placed, when it was inserted, and when it was removed.
- Documentation alone will not absolve or find liability. Rather, the documentation needs acceptable legal support from expert witnesses, occurrence witnesses and radiographic evidence, as examples.
- Res Ipsa Loquitor is a legal doctrine that often applies to retained surgical bodies cases.
- Rather than just treat if a wound does not heal, investigate the cause, as discussed in our blog “Wound Detective Series: When Wounds Won’t Heal.
Learn more in our Skin and Wound Management Course.
What do you think?