Wound pain is sometimes difficult to quantify, but if a patient complains of pain, this requires effective and timely pain management. In the midst of the war on narcotics, that might mean looking for alternative pain management techniques and learning new approaches.
Several months ago, I was attacked by the most venomous scorpion in North America, the Arizona bark scorpion. This stealth attack happened while I slept in my own bed at home in our southern Nevada desert home. I woke up with a jolt knowing that something was terribly wrong with me, but not quite sure what was happening. I felt a fiery tingling pain in both my hands and my abdomen, yet at the same time I also had a total loss of feeling in those areas. I remember yelling to my family that I was paralyzed, but they were confused because I was running around and frantically waving my arms obviously not paralyzed at all. We only figured out what had happened when I tried to crawl back into bed and saw the scorpion on my pillow.
My scorpion stings were an indescribable sensation and unlike any type of pain I had ever experienced. Even today, I am struggling to find the words to tell you what it felt like. All I knew was that it hurt and was unlike any pain I had previously experienced or could even compare it to. For the record, I did some research afterward—people describe it as feeling quite similar to being electrocuted. Luckily, I can say that I was never electrocuted, but that is how people describe it.
Just as luckily, I have never had a pressure injury or a diabetic foot ulcer, so I am not really sure what those feel like either. My patients tell me they hurt. Some patients seem like they are in extreme pain, while others seem to have only mild pain. How do we quantify wound pain, and more importantly, how do we manage it effectively?
The Wounds Do Not Hurt Myth
Over the years, I have heard many healthcare practitioners (HCPs) say that pressure injuries and diabetic foot ulcers do not hurt. This always puzzled me because they certainly look like they hurt. This myth probably started because people who develop a wound often have paralysis or nerve damage and are unable to feel the painful situation developing. This is the precise reason why we tell patients with diabetes to inspect their feet daily just in case they are developing an ulcer they cannot feel.
While loss of sensation is a contributing factor to wound development, I am not certain we can conclude that the wound itself does not hurt. If you have ever witnessed a debridement session or a dressing change even on a paralyzed patient, you probably have noticed some wincing and moaning. Did you continue the treatment or stop and address the wound pain?
Suing for Pain and Suffering
Every state has different rules about including pain and suffering in a lawsuit. Whether or not pain and suffering claims become an official part in a lawsuit is for the attorneys to work out. What HCPs need to understand is the poor impression it leaves when family members and loved ones describe how their dear mother or beloved spouse was allowed to writhe in agony.
Family stories carry weight, and it is always difficult to hear that they thought the medical care they received was unsympathetic and blind to their pain. When a credible patient or their family member describes what ensued when pain management was not handled to their satisfaction, it often makes me cringe. And it often contributes to hefty out-of-court settlements. I have seen family members resort to bringing in their own pain medication because loved ones of 90-year-old nursing home patients begging for relief were denied medication because it was “not time yet” and others offhandedly were told that the medication “should have worked.” What type of impression do you think these memories make?
Measuring Suffering
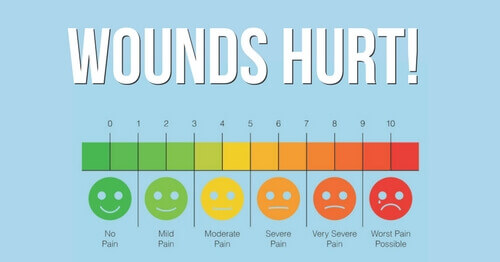
Just as I cannot effectively describe to you what it felt like for me to be stung by a scorpion, patients each experience pain unique to themselves. Pain is impossible to see. We can see the wound, but we cannot see the wound pain. How do you measure something you cannot see? In many cases we rely on the good old-fashioned pain scale ranging from 1 to 10, with 1 meaning free of pain and 10 meaning the most pain imaginable. In this digital age, it is hard to comprehend that this is the best we can do, but depending on the care setting, it often is. This becomes even more of a problem when dealing with cognitively impaired patients who might not understand the scale at all.
Adjusting the Narcotics or Nothing Approach
The opioid crisis and the war on drugs certainly has changed the pain management landscape. This does not negate the fact that patients still need their pain managed effectively. If a patient tells you his or her wound hurts and the treatment hurts, you must address this until the patient is satisfied. Pain is taxing physically, as well as emotionally.
If the medical profession is to reach the goal of reducing narcotic usage, we are going to have to come up with viable alternative solutions. Ignoring wound pain is simply not an option. Many integrative pain centers are getting good results with acupuncture, yoga, meditation, acupressure, massage, and other non-drug techniques. In addition, a total of 29 states, the District of Columbia, Guam, and Puerto Rico now allow for comprehensive public medical marijuana and cannabis programs.1 Cannabidiol (CBD) oil is a non-psychoactive option that many people have used with positive results for a variety of conditions, ranging from managing seizures to managing chronic pain.
Crafting the Future
The conundrum I come across is that many HCPs I work with are resistant to these treatments because they consider them fringe approaches. They do not want to give opioids and narcotics, but might think acupressure is a joke, yoga is for hippies, and CBD oil is for stoners.
My questions for discussion are twofold. Have you had success with any of these techniques? The best way these treatments will get into the mainstream is by talking about success stories and encouraging others to try something they might not have considered in years past. And have you vowed to become more attentive to pain management? You do not want to hear the lawyer describe you as someone who was indifferent to another human’s suffering. The reality is one day we will all suffer some sort of pain, and we should all give the care we would wish for ourselves and our own loved ones.
Reference
- National Conference of State Legislatures. State medical marijuana laws. National Conference of State Legislatures website. https://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Published February 15, 2018. Accessed March 5, 2018.
Wound Care Education Institute® provides online and onsite courses in Skin & Wound, Diabetic and Ostomy Management. Eligible clinicians may sit for the prestigious WCC®, DWC® and OMS national board certification exams through the National Alliance of Wound Care and Ostomy®(NAWCO®). For details, see wcei.net.
What do you think?