To treat patients with lower extremity ulcers, you need to find out if there’s impaired arterial blood flow. For some patients, however, the standard Ankle Brachial Index (ABI) yields misleading results. Fortunately, there’s an easy alternative: the Toe Brachial Pressure Index (TBPI). Here’s when and how to perform this simple test.
When confronting a lower extremity ulcer, we know that the usual wound assessment isn’t enough. Standards of care guide us to perform an Ankle Brachial Index (ABI) to calculate blood flow. By doing so, you can rule out significant arterial disease and determine the amount of venous compression you can safely apply.
The ABI compares the systolic blood pressure of the ankle to that of the arm (brachial) with the following formula:
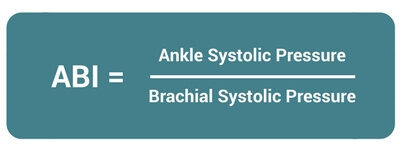
Values between 0.41-0.91 represent peripheral arterial disease (PAD) sufficient to cause claudication. Meanwhile, values of 0.00-0.40 reflect severe PAD sufficient to cause resting pain or gangrene. Refer the patient to a vascular specialist for further assessment.
When the ABI Falls Short: Hardened Arteries
If your patient has a long history of diabetes, severe neuropathy, or kidney disease, the ABI diagnostic may yield misleading results because of calcified arteries. In other words, If the blood pressure cuff cannot adequately compress the arteries, your ABI will be falsely inflated.
If you already know your that your patient has calcified arteries or an ABI comes back with an abnormally high value (>1.3), you need an alternative approach. That’s where the Toe Brachial Pressure Index (TBPI) enters the picture.
How to Perform a Toe Brachial Pressure Index
The Toe Brachial Pressure Index is a non-invasive method of determining blood flow through the arteries in the feet and toes, which seldom calcify. The procedure resembles the more familiar ABI. If you have solid blood pressure skills, you will master the TBPI with ease.
TBPI Equipment
First, gather the items you’ll need on hand to complete the TBPI measurements:
- A blood pressure meter with an arm cuff and toe cuff
- A handheld Doppler ultrasound device
- Ultrasound transmission gel
- Tissue or gauze
- Damp cloth or alcohol wipes
Measuring Brachial Systolic Pressure
- Have the patient remove shoes and stockings and lie down for at least 10 minutes prior to obtaining blood pressure measurement.
- Apply the blood pressure cuff snugly on the upper arm with the lower edge of the cuff 1 inch above the antecubital fossa (pit of the elbow) and palpate for the brachial pulse.
- Apply conductivity gel over the brachial artery. Turn on the Doppler device and place the tip of the probe at the antecubital area at approximately a 60-degree angle to the surface of the skin.
- Move the probe around until you hear the clearest arterial pulse sounds. Keep the probe at that position.
- Inflate the blood pressure cuff to approximately 20mm Hg above the numerical reading where the pulse sounds cease.
- Slowly deflate the cuff at a rate of 2 mm Hg per second until you hear the first arterial pulse sound. When this number is determined, deflate the cuff completely and record this systolic reading.
- Remove the gel from the patient’s skin with a tissue or gauze
- Repeat the procedure in the other arm and record the reading.
Measuring Toe Systolic Pressure
- Place the toe cuff around the base of the great toe. Use the second toe if the great toe can’t be used.
- Palpate the pulse signal on the toe’s distal pad area. Apply transmission gel to the pulse site.
- Place the tip of the Doppler probe onto the gel at a 45-degree angle to the skin surface. Direct the probe toward the patient’s head to detect the pulse signal.
- Slowly inflate the toe cuff until you no longer hear the pulse signal (to a maximum of 200 mm Hg). A partial squeeze should adequately inflate the cuff.
- Slowly deflate the toe cuff until the point at which the pulse signal returns. This is the toe’s systolic pressure.
- Remove the toe cuff. Use tissue or gauze to remove the leftover gel from the patient’s skin and from the Doppler probe. Gently clean the Doppler probe with a damp cloth or alcohol wipe.
- Calculate and document the results with the Toe Brachial Pressure Index formula, using the brachial systolic pressure in the arm with the highest pressure:
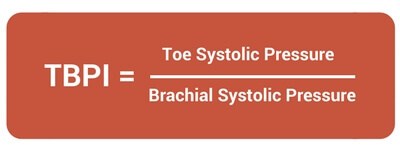
Understanding Toe Brachial Index Results
How do you interpret the number that results from your measurements and calculation?
TBPI > 0.7 Normal, suggests no arterial disease
TBPI = 0.64 – 0.7 Borderline
TBPI < 0.64 Abnormal, suggests arterial disease
If the absolute Toe Pressure (mm Hg) ≤30, this indicates Lower Extremity Arterial Disease and predicts a failure to heal.
Do you already see widespread adoption of the ABI and the TBPI in your facility? If so, do you have any handy tips for your fellow clinicians? Can you offer recommendations for your favorite equipment? We welcome you to share your knowledge and help elevate the skills of your fellow healers.
Wound Care Education Institute® provides online and onsite courses in Skin, Wound, Diabetic and Ostomy Management. Eligible clinicians may sit for the prestigious WCC®, DWC® and OMS national board certification exams through the National Alliance of Wound Care and Ostomy®(NAWCO®). For details, see wcei.net.
DISCLAIMER: All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to the care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.
What do you think?