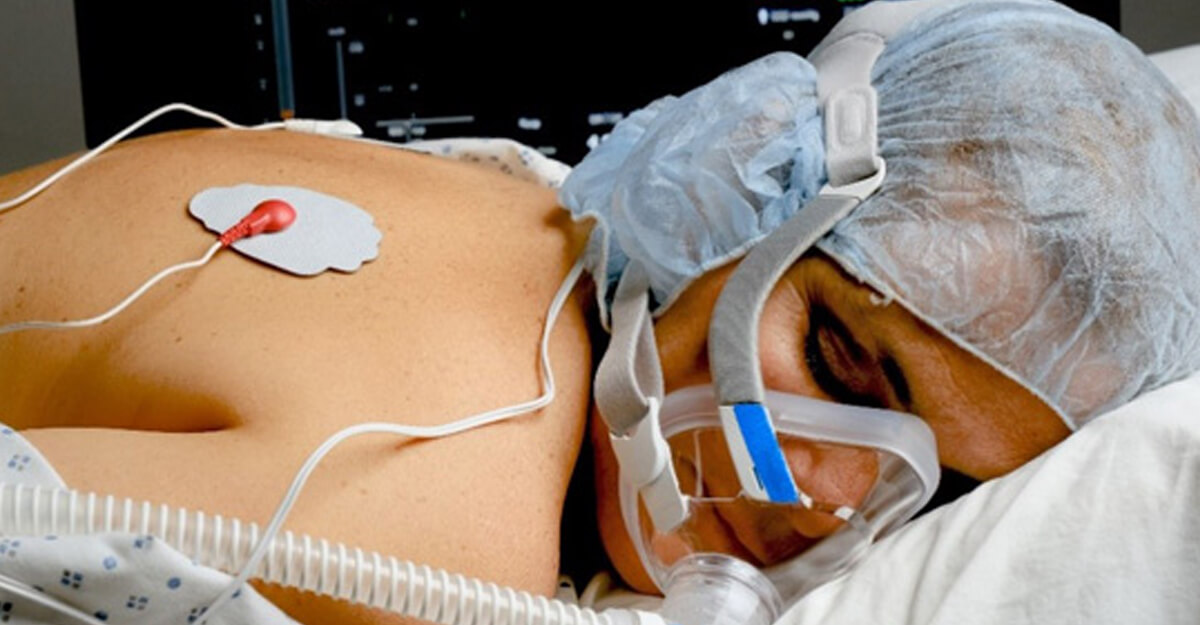
As the COVID-19 pandemic endures, there is an increased awareness of the practice of placing patients in prone positioning versus supine positioning.
Prone positioning is important when patients are experiencing acute respiratory distress syndrome (ARDS), which is a risk for those who have the virus.
Prone therapy is not new, however.
“Critical-care nurses have known for many years that prone positioning patients with ARDS results in lower mortality rates and less incidence of lung injury,” said Kathleen M. Vollman, MSN, RN, CCNS, FCCM, FCNS, FAAN, clinical nurse specialist and consultant at Advancing Nursing, LLC.
Prone therapy was a nursing intervention first used personally by Vollman on an ARDS patient in 1981.
“In 1970, ARDS had a 70% mortality rate,” she said. “I was an early adopter of using the prone position after reading the results of two small studies at the time. Proning is a non-invasive maneuver that nurses own.”
Vollman pointed out patients need to be placed in the prone position earlier rather than later during the course of ARDS, and for several hours — 12 to 16 out of 24 — for outcomes to improve.
How prone positioning therapy works
Patient outcomes improve and mortality rates drop for ARDS patients placed in the prone position, according to Vollman, for the following reasons:
- More homogenous, consistent aeration of the lung in ARDS, which reduces regional shear strain and less ventilator-induced lung injury (VILI)
- Increased oxygenation
- Improved dependent aeration recruiting alveoli
- Reduced hyperinflation of nondependent regions
- Decreased barotrauma and atelectrauma by recruiting and reducing overdistension that occurs with higher positive end-expiratory pressure (PEEP)
- Lower PACO2 relates to a net increase in recruitment of alveoli and a decrease in dead space
- Helps to drain secretions
- Shifting of lung water and densities
On the flipside, when patients are placed and kept in the supine position, it results in poor patient outcomes and increased morality rates. Why?
Vollman said the supine position causes a significant reduction in lung volumes; alteration in the lung mechanics, resulting in low compliance and high resistance; alveoli to collapse, causing compression atelectasis; and hypoxemia.
As with any therapy, there are specific criteria to adhere to regarding which patients can be placed in the prone position. Vollman said these are patients with severe ARDS (PaO2/FiO2 <150 mmHg); per ATS/SCCM Mechanical Ventilation for ARDS guidelines, a strong recommendation for prone positioning for more than 12 hours per day and patients early in the course (12-24 hours).
Although prone therapy is highly effective at decreasing the rates of lung injury and mortality in ARDS patients, there are some patients who should not be placed in a prone position, Vollman said. These are patients with:
- Facial trauma, neck trauma or spinal instability
- Recent sternotomy or large ventral-surface burn
- Massive hemoptysis
- Elevated intracranial pressure
- High risk of needing CPR or defibrillation
Additional contraindications for using prone therapy are listed here.
Risk for pressure injuries
Healthcare professionals are fully aware of the multiple factors that contribute to the increased risk for avoidable and unavoidable pressure injuries (PIs) developing in various patient populations, and especially in those who are immobile and critically ill.
The risk factors for developing a PI are older age, use of vasopressors, altered mobility, impaired tissue oxygenation, impaired tissue perfusion and length of stay in the critical-care unit.
Among the many factors that can raise patients’ risk for developing PIs, being in a single position for a length of time is one of them. Using the prone position is no different.
“Specific nursing interventions need to occur to reduce patients’ risk,” Vollman said.
While HAPIs can occur in any location, there are several pressure injury points on the ventral side of the body that are susceptible to PIs when proning patients, according to experts. These include the forehead, cheeks, nose, chin, clavicle, elbow, chest/breasts, genitalia (penis), anterior pelvic bones, knees and feet (dorsum area).
Strategies to prevent pressure injuries during prone positioning
There are three important ways to help prevent PIs from forming in proned patients.
1. Microshifts
First, perform microshifts (small position changes) while proned, especially in non-rotating beds.
2. Manual proning
Secondly, with manual proning, shift and reposition the patient’s head every two to four hours, or as clinically indicated.
3. Assess all pressure points
Finally, assess all pressure points by:
- Assessing anterior surfaces before proning and assessing posterior surfaces before returning to the supine position
- Checking the skin integrity of the arms, head and face when alternating from the arm position to the swimming arm position
- Documenting all skin assessments and preventive measures
To prevent pressure injuries in proned patients using prophylactic dressings, apply soft silicone prophylactic multi-layered foam dressings to pressure points and offload and protect the chest and breasts, trunk, genitalia (areas that are particularly sensitive in prone the position).
In addition, clinicians should avoid applying multiple layers of dressings, which will increase pressure. Assess dressings, and regularly peel them back, to check the skin underneath while supine and follow each product manufacturer’s instructions.
Moisture management is essential and can be ensured by:
- Using liquid skin protectants and sealants on the face
- Changing foam dressings PRN
- Applying hydrofiber/calcium alginate dressings under prophylactic dressings to manage excess moisture
- Securing all medical devices and tubes away from the skin
- Assessing and protecting the surrounding skin with thin, prophylactic dressings and bridge areas with positioning devices
Importance of offloading
Devices can be used to offload the head and feet.
For the head, consider foam density, cushion height, face angle and endotracheal tube (ETT) positioning when selecting the appropriate device.
Commercially available ETT securement devices might contribute to increased skin breakdown in prone patients, so consider tape to secure ETT while proning.
Create channels for tubes with positioning aids, and ensure no unsecured devices are placed under the torso or legs.
Align urinary catheter and fecal management devices toward the foot of the bed.
For more information about a safe prone positioning checklist while managing ARDS patients, visit this site.
Learn more about preventing pressure injuries, in our webinar series on the subject!
What do you think?