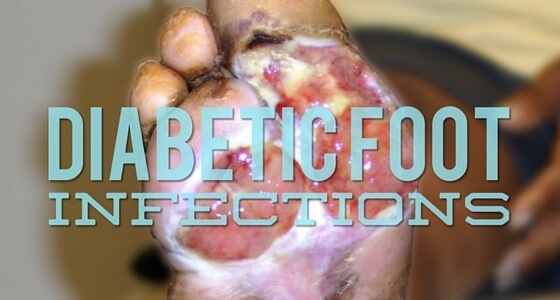
For effective diabetic wound management, clinicians must know the risk factors for foot infections, and be able to diagnose them properly – and as soon as possible.
Wound care clinicians deal with foot infections all the time, but when the patient is also diabetic, an infection can progress rapidly to a critical state. In fact, it is estimated that around 56% of diabetic foot ulcers become infected, and an infected foot wound precedes about two-thirds of amputations. Being able to treat diabetic foot infections promptly – before they progress too far – helps prevent amputations, which is why your role is so crucial to a patient’s well-being.
What are the risk factors of diabetic foot infection?
If you are treating a diabetic patient with a foot infection, there are a number of risk factors to consider. These include:
- 30-day-old wounds
- Wounds that go down to the bone
- Recurrent foot infections
- Peripheral vascular disease
- An etiology from trauma
In particular, be on high alert with your diabetic patients for what they call an occult (hidden) infection. A diabetic foot ulcer could clearly have an infection, but fail to show any of the classic signs and symptoms that you traditionally look for, like erythema, heat, pain and purulence.
Because a diabetic patient’s immune system is compromised, you might be on the lookout for typical signs but not see any of them at all. This does not mean that an infection isn’t there; only half of diabetic foot ulcer patients will show classic signs, which means we also need to work our patients up for infection.
The best approach? Be persistent and keep looking for more signs, like:
- Serous exudate (thin, clear, watery)
- Delay in healing
- Friable (fragile) granulation tissue
- Discolored granulation
- Odor
- Pocketing in the wound bed
How do we diagnose diabetic foot infection?
Diagnosing infection in any wound, particularly with diabetic patients, is a clinical one (versus a lab diagnosis). So if you ever hear a colleague say, “We’re going to wait for the lab results to see if our patient has a wound infection,” it’s time to stand up and emphatically say, “No!” Why? Because lab results, specifically the swab cultures that are most commonly used, are often inconclusive in the presence of biofilm. Instead of waiting for the results, you need to act immediately.
That’s not to say that lab results aren’t useful. They can sometimes help us confirm infections and target which antibiotic we want to use. But again, most infections are polymicrobial (containing more than one kind of bacteria), and swab cultures don’t pick up everything. We need to use our clinical judgment and supplement with lab and cultures.
The final word
As wound care professionals, prevention is obviously our first line of defense against any wound complications from infections. But when caring for diabetic patients, clearly understanding the risk factors for foot infections, and then being able to diagnose conditions as soon as possible, are crucial for effective treatment.
What do you think?
Have you had experience in treating diabetic patients with foot infections? Have you been able to identify the infection in a timely manner? Is there a particular case that was exceptionally challenging or difficult? Please tell us about it, and leave your comments below.
What do you think?