Proper assessment is essential for differentiating between venous and arterial ulcers.
Your patient has a lower extremity wound. You aren’t sure what exactly you are dealing with. You know you need to measure the ankle-brachial index (ABI), but as you wait for results, some of your wound assessment findings offer clues.
Characteristics of Venous Ulcers
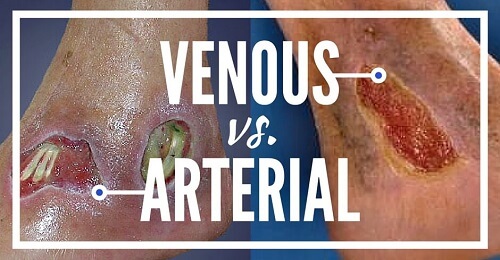
Let’s start with the venous ulcer, typically found on the medial lower leg, medial malleolus and superior to the medial malleolus. Seldom will you see them on the foot or above the knee. They tend to be irregular in shape, are superficial, have a red wound bed, have moderate to heavy amount of exudate and the patient may have no pain or a moderate level of pain. Surrounding skin can be warm to the touch, edematous, scaly, weepy and you may see hemosiderin staining present. An ABI provides a definitive answer and will come back at 0.9.
Characteristics of Arterial Ulcers
You will typically find an arterial ulcer on the lateral malleolus, over the phalangeal heads, between the toes, tips of toes or areas that are subject to trauma and rubbing. They tend to be regular in shape, round punched out in appearance. Deep pale wound beds with necrotic tissue present are common in the arterial patient. The wound will likely produce minimal exudate, and the patient will complain of extreme pain. The pain typically starts out as intermittent claudication or cramping in the lower extremities and then continues to progress. Surrounding skin will be cool to the touch, pale, cyanotic, hairless on ankle and foot with thickened toenails. Finally, the ABI will come back abnormal and low at 0.5, indicating significant arterial disease.
Mixed Venous and Arterial Ulcers
Unfortunately, sometimes the answer isn’t so clear. The patient with a lower extremity ulcer may present with signs and symptoms of both arterial and venous issues. You may see a full thickness wound, irregular in shape with minimal exudate on a cool pale lower extremity. What then? Then we go back to the gold standard of bedside tests, our ABI to determine what we are dealing with for sure. When the etiology is mixed, most likely the patient’s ABI will fall somewhere between 0.6-0.8.
The Importance of the Ankle-Brachial Index (ABI)
Our assessment skills can help guide us in differentiating these lower extremity wounds. But remember, not every ulcer always follows the rules. For example, it is possible to find a venous ulcer on the lateral side. This is why ultimately, the ABI is the gold standard of care and must be done to rule out arterial disease. Move beyond the excuses: we always need to do a full comprehensive assessment, and one that includes the ABI for our patients with lower extremity wounds.
How to Remember the Difference
Do you struggle to remember the differences between venous and arterial ulcers? Luckily, we have a system that will help you keep it all straight. See Venous vs. Arterial Ulcers: What’s the difference? for details.
Wound Care Education Institute® provides online and onsite courses in the fields of Skin, Wound, Diabetic and Ostomy Management. Eligible clinicians may sit for the prestigious WCC®, DWC® and OMS national board certification examinations through the National Alliance of Wound Care and Ostomy® (NAWCO®). For more information, see wcei.net.
What do you think?