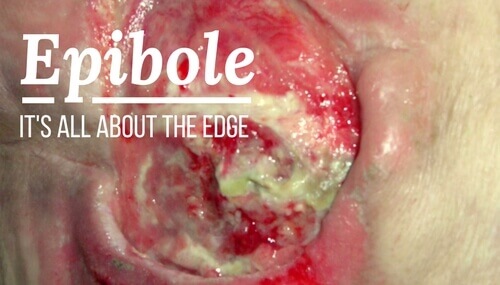
How do you spot an unhealthy wound edge? Learn more about the causes, prevention and treatment of epibole.
When it comes to treating epibole, it’s all about knowing what a healthy wound edge looks like – and being able to spot signs of trouble. This basic overview includes epibole causes, prevention and treatment. We’ll have you ready to meet this condition head-on and get your patients on their way to recovery.
The Ideal Wound Edge
Let’s take a look at what happens as full-thickness wounds heal. First, they begin to fill in from the bottom upward with granulation tissue, which is the deep, beefy-red tissue that replaces dead tissue in healing wounds. Meanwhile, wound edges contract and pull together, with movement of epithelial tissue (cells in the top-most layer of the epidermis), toward the center of the wound (contraction). These epithelial cells, arising from either the wound margins or residual dermal epithelial appendages within the wound bed, begin to migrate across the wound bed in leapfrog (or train) fashion. Horizontal movement stops when cells meet (contact inhibition).
So, what is the ideal wound edge? It will be:
- attached to and flush with the wound bed
- moist and open with the epithelial rim thin
- pale pink to translucent
What Is Epibole?
In many chronic wounds, a problem with slow or absent epithelial edge advancement is caused by the clinical condition we know as epibole. Epibole refers to rolled or curled-under closed wound edges. These rolled edges may be dry, callused, or hyperkeratotic (a thickening of the epidermis, the outermost layer of the skin). Epibole tends to be lighter in color than surrounding tissue, have a raised and rounded appearance, and may feel hard and rigid.
Causes of Epibole
When the upper epidermal cells roll down over the lower epidermal cells and migrate down the sides of the wound instead of across, the result is epibole. Edges that roll over ultimately cease migration once epithelial cells of the leading edge come in contact with other epithelial cells on the sides of the wound. In other words, the body thinks the wound is healed and epithelial migration across the top of the wound ceases.
There are many possible reasons why the epidermal margin fails to migrate, including:
- hypoxia (deficiency of oxygen reaching the tissues)
- infection
- desiccation (extreme drying out)
- dressing trauma
- an over-packed wound bed
- an unhealthy wound bed
- the inability to produce the basement membrane for the epithelial cells to adhere to
- cellular senescence (the inability of cells to divide/proliferate)
Epibole Prevention
So how can you prevent epibole? Follow these tips:
- Pack dead or empty space in the wound bed. Packing promotes healing from the bottom up, and avoids abscess formation at the wound depth. For more information, check out the video How to Pack a Wound.
- Fill the depth of the wound to the surface. Do not pack tightly, as this will cause pressure and impair circulation. Wound fillers, hydrogel impregnated gauze, alginates or fluffed plain-woven moistened gauze can be placed loosely into the space.
- Protect periwound skin with a skin sealant, moisture barrier ointment or barrier wafer.
- Prevent epidermal stripping by using silicone border dressings or silicone tape. Consider tape-free strategies for securing dressings.
- Protect the wound from pressure.
Epibole Treatment
Treatment for epibole involves reinjuring the edges and opening the closed tissue, which renews the healing process. Options include:
- conservative or surgical sharp debridement
- treatment with silver nitrate
- mechanical debridement by scrubbing the wound edges with monofilament fiber dressings or gauze
For more information about treating epibole, download our free Wound Bed Interventions guide.
Are You Epibole Ready?
How often do you encounter epibole in your facility, and are you confident in your ability to see the signs and treat it? Have you found that taking preventative measures has impacted the frequency of this condition? Please share any thoughts or ideas you have about this topic by leaving your comments below.
Wound Care Education Institute® provides online and onsite courses in the fields of Skin, Wound, Diabetic and Ostomy Management. Eligible clinicians may sit for the prestigious WCC®, DWC® and OMS national board certification exams through the National Alliance of Wound Care and Ostomy® (NAWCO®). For details see wcei.net.
What do you think?