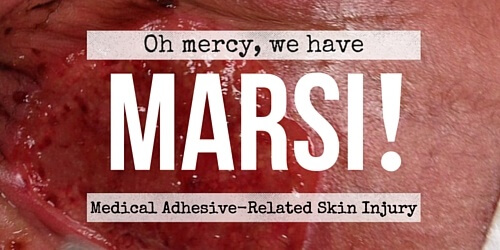
If you practice wound care, here’s what you need to know in order to avoid Medical Adhesive Related Skin Injury – also known as MARSI.
Here’s a quiz for all of you in wound care: how many medical adhesive injuries are reported each year in the United States? The answer is 1.5 million. That’s a lot of skin tears and other painful dermal injuries that might have been prevented.
The good news is that with continued education, we can all help decrease Medical Adhesive Related Skin Injury (MARSI). This new descriptor in skin injury is definitely something you need to know.
The State of MARSI
The Health Care Reform Act mandates that we mitigate pain and upgrade our care habits to provide the safest care possible. Not only is this good for patients, it’s also good for facilities. In 2012, about $850 million in payments to hospitals were withheld because of MARSI. Fortunately, hospitals have the opportunity to recoup those monies with high satisfaction scores from patients, based upon better pain management.
Some of you might be thinking, “Really? How hard is it to remove a dressing or electrode?” The reality is that many of the newer adhesives used in wound care are stronger than ever, in order to overcome the issues of non-adhesion due to in- continence, effluent, or wound exudate. This strength, along with incorrect removal of the adhesive tape, can result in MARSI.
What are Medical Adhesive-Related Skin Injuries (MARSI)?
MARSI is defined as a medical-related skin injury in which erythema and/or other manifestation of skin trauma or reaction including formation of vesicles, bulla, skin erosion, and epidermal tears, persist longer than 30 minutes after removal of the adhesive tape. Other injuries include contact dermatitis and tension injuries from allergy, or tape applied too tightly or stretched over the skin.
Who is at Risk for MARSI?
Wound care can be stressful as it is, and having so many types of medical tapes to choose from – and so little time for dressing changes – can add to the mix. It’s not always easy to know which adhesive works best for the job in front of you, keeping in mind that we need our adhesive dressings and ostomy supplies to adhere and remain in place for 2-7 days. And while we mean well, sometimes the tape removal process doesn’t go as planned.
It’s important to first be aware of the type of patients that are more disposed to skin injury. Who is most at-risk?
- The elderly with age-related dermal fragility
- Infants in the NICU with under-developed epidermis
- Patients with a diagnosis of malnutrition and dehydration
- Those with moisture and incontinency
- Patients on medications such as corticosteroids and radiation
- Patients with dermal pathology, such as eczema.
Wound Care Tips for Avoiding MARSI
Knowing who is particularly vulnerable to MARSI is crucial, as is choosing the right tape for the patient’s condition and specific wound goals.
General rules of thumb
- The newer foam and silicone tapes are more gentle to the skin.
- While cloth tape adheres most strongly, it can tear the skin.
- Tapes with stretch ability are excellent to go over joints and areas prone to edema.
- Consider use of tubular netting /gauze to secure dressings in place rather than tape if skin is compromised or fragile.
The dressing and tape manufacturer can provide information on the use of their products, with specific instructions regarding how to avoid trauma. In addition, clinicians can reduce MARSI with the proper application and removal of adhesive dressings.
Helpful tips
- Prepare the skin by cleansing and drying gently, trimming and shaving hair as necessary. Apply skin sealant prior to dressing placement.
- Briefly holding the tape or dressing in place – the pressure and warmth of the hand help secure the adhesive.
- Do not tape a limb circumferentially and minimize tape tension over all skin surfaces.
- Remove tape “low and slow” in the direction of the hair growth. Keep the tape parallel to the skin and push the skin away from the tape with other hand.
- Remove transparent film dressings by lifting a corner and stretching it horizontally along the skin surface to break the adhesive bond [See video].
- Continue stretching from the edge of the dressing to the center.
- When the two sides are partially removed, grasp both sides. Stretch horizontally and parallel to the skin until the entire dressing lifts.
And remember, if you note any erythema or any trauma, change the type of dressing and apply a gentler type of tape to areas of skin not taped before. Change treatment and application techniques as needed to reduce further MARSI.
MARSI Prevention and Education

Develop MARSI Risk Signage
Wound care and prevention always begin with education. Know more about at-risk patients and proper use of adhesive dressings. As for improved outcomes, they are the result of trauma avoidance and knowing when to change course, including having the safer tapes and dressings on-hand and in the formulary. In addition, just as we have increased awareness of patient fall risk through signage and educational initiatives, perhaps we should develop signage for MARSI risk patients. With heightened awareness and proper care, we can reduce the annual number of medical adhesive injuries.
Are You on Board?
Are you or your colleagues making efforts in your facility to use safer tapes and dressings? Have you had particularly challenging cases of MARSI, and what did you do to improve the wounds? If you have any stories to share, or advice on how to treat or avoid MARSI, please tell us about them here. We love being able to learn from each other.
Wound Care Education Institute® provides online and onsite courses in Skin, Wound, Diabetic and Ostomy Management. Eligible clinicians may sit for the prestigious WCC®, DWC® and OMS national board certification exams through the National Alliance of Wound Care and Ostomy®(NAWCO®). For details, see wcei.net
DISCLAIMER: All clinical recommendations are intended to assist with determining the appropriate wound therapy for the patient. Responsibility for final decisions and actions related to care of specific patients shall remain the obligation of the institution, its staff, and the patients’ attending physicians. Nothing in this information shall be deemed to constitute the providing of medical care or the diagnosis of any medical condition. Individuals should contact their healthcare providers for medical-related information.
What do you think?