Eschar is formed when necrotic tissue is present. While this condition can appear as a natural shield for certain wounds, it can severely hinder the course of healing.
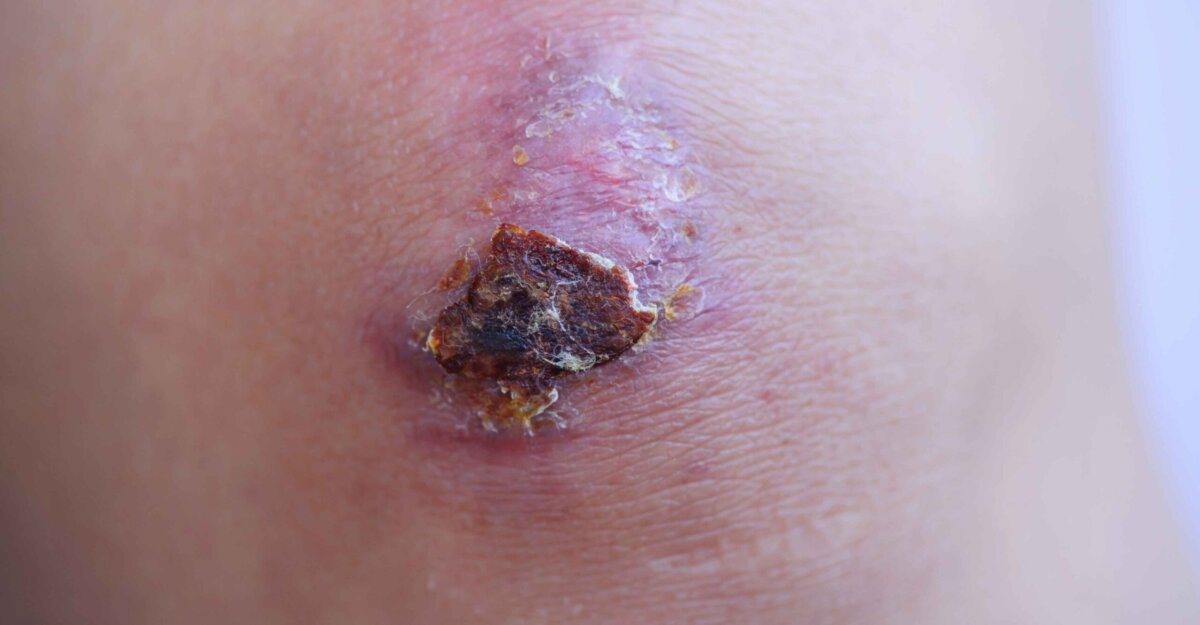
Usually appearing as dark brown or black in color, eschar refers to devitalized tissue found in a wound bed. It is often dry and thick in texture but may present as soft, boggy, or fluctuant.
Boggy, fluctuant eschar is frequently seen in the presence of tissue infection, often in pressure injuries and arterial ulcers. However, it can also be present in wounds of other etiologies if poor blood flow is present.
When navigating this tissue, it is imperative to explore its defining characteristics, causes, and the diverse approaches in treating and preventing this condition.
Eschar vs. scabs
To complete an adequate and thorough wound assessment, it is important to be able to differentiate between eschar tissue and a scab. These two wound characteristics are not interchangeable.
A scab or “crust” is made up of dried blood, cells, and dried serum, often forming on the surface of a recently healed wound. If removed carefully, normal and healthy epithelial tissue will often be revealed underneath the scab. A scab may also form over an unhealed ulcer that has dried out, which can happen if a wound is exposed to air and loses its warm, moist healing environment.
Conversely, eschar is the product of necrotic tissue, which is often seen in a wound with poor perfusion. Because of this, it is not always appropriate to remove this type of tissue.
What causes eschar tissue?
When there is decreased blood flow to an open wound, eschar can form. Its presence can be found in any wound etiology but is most often seen in pressure injuries. This is due to unrelieved pressure causing poor perfusion to the skin.
Once skin loses its blood source, the tissues begin to die. This tissue death results in formation of a wound. Of course, not all pressure injuries will form this, but it is typically seen in deeper, high-staged wounds.
The National Pressure Injury Advisory Panel (NPIAP), noted that this tissue type can appear in Stage Three or Four pressure injuries. Arterial ulcers also commonly present with black eschar due to their poor perfusion. Eschar-covered arterial ulcers may be seen on distal toes and the malleolus.
Open calcaneus wounds are often mixed etiologies of pressure injury and poor arterial blood flow. For this reason, the heel of the foot is a very common area for this tissue to develop. Wound patients who are immobile, smoke, and/or have poor nutritional status may be at a higher risk of developing this tissue.
Full-thickness burns develop eschar due to the level of tissue destruction. Significant burn wounds are most often treated by a specialized burn team. If any of the following burn locations or patient populations experience burns, they should be assessed by a burn team:
- Burns over a large area of the body
- Burns that cover a joint
- Burns appearing on the palms of the hands
- Burns on the soles of the feet
- Older patients
- Very young patients
Treatment options
Treatment usually involves removal of the devitalized tissue though it is not always necessary to remove this tissue.
Dry, stable eschar without surrounding redness may be best left intact to protect the wound from infection. Stable tissue that is lifting at the edges may be trimmed as needed.
However, eschar that has drainage or feels boggy should be removed, as there may be infection developing. If there are other signs of infection present, including odor or surrounding redness, the tissue should be removed.
Removing necrotic tissue will facilitate culture and proper treatment of infection and can be done by autolytic, mechanical, enzymatic, or sharp debridement. A surgical escharotomy may be necessary for full-thickness burn wounds. These are often performed by a specialized burn team or plastic surgeon.
Paths to prevention
Measures to prevent the formation of eschar have the same guidelines as current wound prevention and treatment. For instance, if appearing in a pressure injury, all efforts should be made to prevent Stage One and Stage Two pressure injuries from deteriorating to Stage Three and Stage Four injuries.
The following approaches are all important factors in wound treatment and help in preventing wound deterioration:
- Pressure relief with frequent repositioning
- Appropriate pressure-relieving support surfaces
- Adequate nutrition
- Hydration
- Reestablishing blood flow when indicated
- Smoking cessation
- Diabetes management
Eschar is not an uncommon occurrence in full-thickness wounds. And when determining appropriate treatment, a thorough assessment can give wounds the safest and most effective path to healing.
If you're interested in expanding your knowledge of wound care, networking with colleagues, or seeing the latest wound care products and technology, register for the Wild on Wounds (WOW) conference August 14–17 in Phoenix, Arizona.
Register NowWhat do you think?